Stuart Brown

Mid-Staffs NHS Foundation Trust was a significantly challenged Acute services provider. The Trust had a very high profile due to concerns raised in 2008 (the Mid-Staffs scandal) about the high rates of mortality at the Trust. The Healthcare commission began an in-depth investigation. Released in March 2009, the report severely criticised the Trust’s management and detailed the appalling conditions and inadequacies at the hospital. Stuart Brown was engaged by the Director of Finance as the Programme Director- June 2010 just as the Public Inquiry led by the eminent Robert Francis QC was starting.
The scandal came to national attention because of an investigation by the Healthcare Commission in 2008 into the operation of Stafford Hospital.
The commission was first alerted by the ‘apparently high mortality rates in patients admitted as emergencies’. When the Trust, failed to provide an adequate explanation, a full-scale investigation was carried out. Released in March 2009, the commission’s report severely criticised the Foundation Trust’s management and detailed the appalling conditions and inadequacies at the hospital. Many press reports suggested between 400 and 1200 more patients died between 2005 and 2008 than would be expected for the type of hospital.
As a result, the trust’s chief executive, Martin Yeates, was suspended, while its chairman, Toni Brisby, resigned. Both Prime Minister Gordon Brown and Health Secretary Alan Johnson apologised to those who suffered at the hospital. Also in response to the
scandal, the mortality rates of all National Health Service hospitals have been made accessible on a
website.
On 21 July 2009, the Secretary of State for Health Andrew Burnham announced a further independent
inquiry into care provided by the Trust. The report made 18 local and national recommendations.
On 9 June 2010 the Secretary of State for Health, Andrew Lansley MP, announced a full public inquiry into the role of the commissioning, supervisory and regulatory bodies in the monitoring of the Trust.

By June 2010 the Trust looked very different in terms of it’s executive management team. Antony Samara had been appointed as Interim Chief Executive and Darren Cattell as the Interim Director for Finance and Performance – both with a track record of turning challenged organisations around and restoring public confidence.
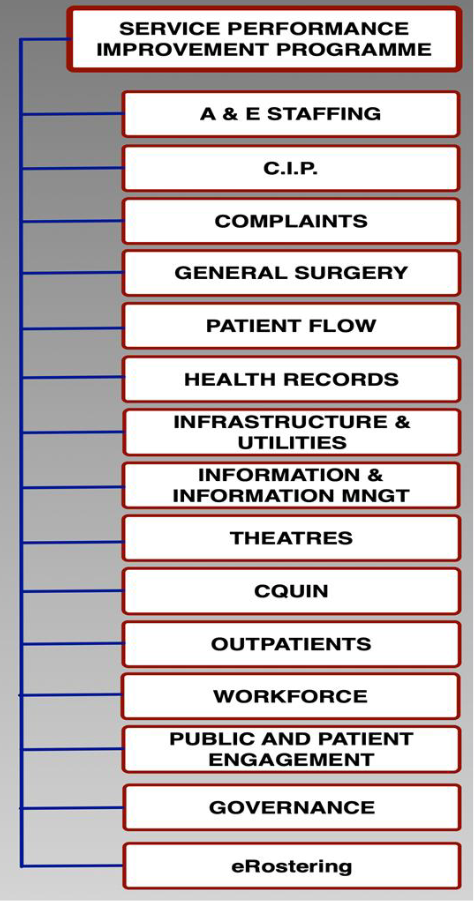
Stuart Brown was commissioned to develop an improvement plan, to be known as the Service Performance Improvement Plan (SPIP) and establish a Programme Management Office at the Trust.
The Trust then had no Programme Management Office functionality, Capability or PMO expertise.
The first issue was to establish the key areas of improvement that would be needed. Then the content of the SPIP would be determined.
The SPIP portfolio is contained in Figure 1.
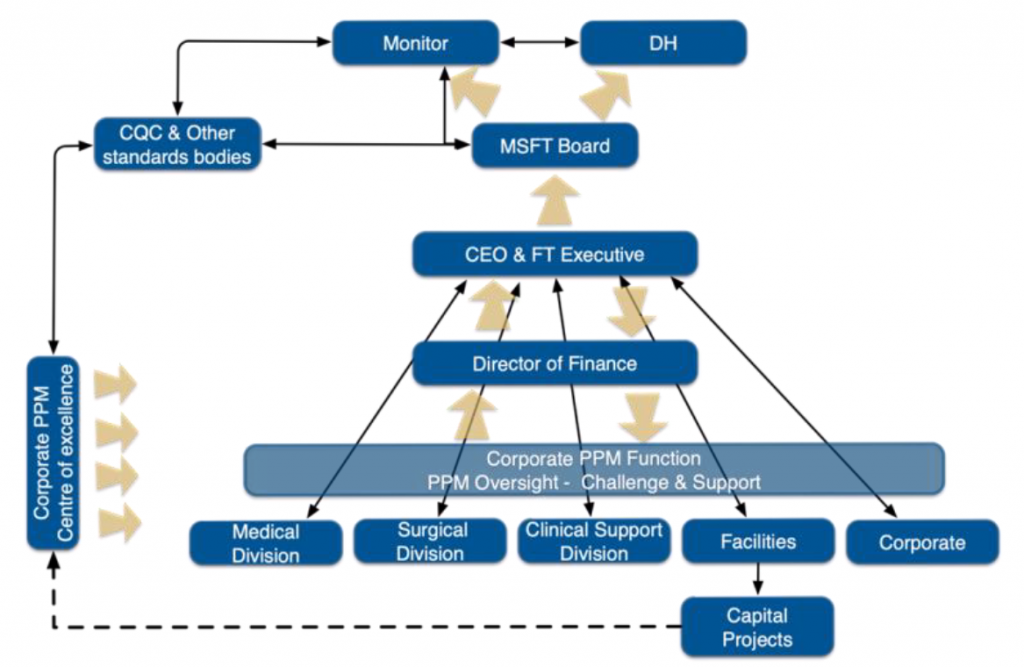
The building of the PMO structure and capacity so to be able to facilitate and drive delivery could then begin.
As there was no recognised programme or project management expertise within the Trust, the team were looked externally for additional expertise and capacity. This was necessary for some of the larger programmes such as Theatre’s and the development of the Cost Improvement Programme which was needed to link to the SPIP in order to manage interdependencies.
Rapid progress was made in the establishment of the PMO and the development and implementation of the Governance structures – figure 2 describes the Governance Structure around the SPIP and the SPIP PMO at Mid Staffordshire NHS FT implemented in June 2010.
As previously stated the Trust had little or no expertise and capacity, so Atos were engaged to help with a
significant diagnosis of the state of the theatre efficiency. The result revealed that the Trust had considerable inefficiency within the suite of Theatre’s which if reduced or eliminated would yield
considerable benefits – both financial and in terms of patient flow through the hospitals and delivery of the Trust’s RTT.
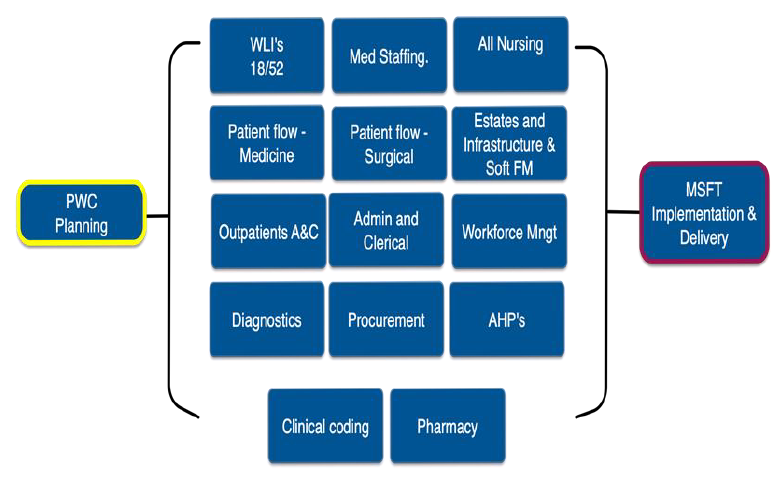
Whilst improving overall quality and performance of the Trust in clinical areas and corporate areas and functions was a critical element of the SPIP objectives managing within means was also seen as a critical success factor (CSF). External pressures to deliver the former meant that the CIP was becoming even more important that it might have been.
The challenge for the Director of Finance and the Programme Director was one of capacity to develop the required programme of work for the CIP.
The decision was therefore taken to engage additional external support, in the form of PwC, to help with the definition and development of the CIP programme. At the same time the capacity was increased within the PMO to support the delivery stage. Figure 3 describes the key themes of the CIP.
Although the Trust did not have spare capacity in terms of personnel who could be seconded to the PMO full time, they were able to tap into a number of internal talented people to support and deliver some of the programmes that formed part of the SPIP.
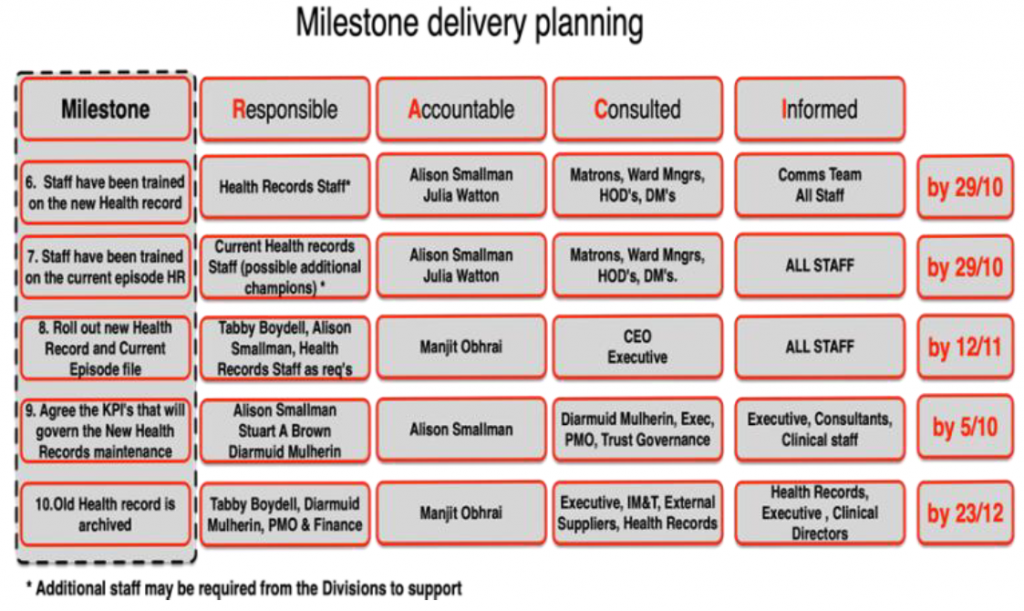
For example, ‘the Health records programme’ where the departments management team was used, supported by a project manager seconded to the PMO, to deliver the rollout of the new type health record and to deliver the associated training required to embed the change over to the new system.
The programme was a complex initiative requiring substantial clinical engagement and delicate stakeholder management because of differing opinions about what should be retained in the Health Record and how long for.
A robust Prince2 based approach was used to project planning including the RACI matrix for milestone planning (see Fig 4). The detailed plan and supporting
documentation was presented to the Board who gave quick approval presentation.